Powassan Virus Overview
What is Powassan Virus? Powassan virus (POWV) is a rare but serious tick-borne viral infection that can be transmitted to humans through the bite of an infected tick, primarily the black-legged or deer tick (Ixodes scapularis) and the groundhog tick (Ixodes cookei). First identified in Powassan, Ontario, in 1958, the virus is named after the location where it was discovered. Unlike other tick-borne infections, such as Lyme disease, Powassan virus is a flavivirus, related to other viruses like West Nile and Zika. It is predominantly found in the northeastern United States, the Great Lakes region, and parts of Canada.
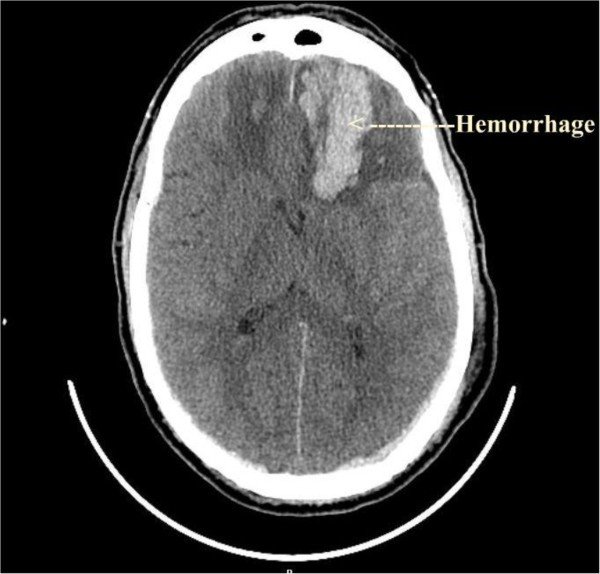
POWV is concerning due to its potential to cause severe and sometimes life-threatening neurological symptoms, as it can infect the brain and surrounding tissues. Powassan virus infections have increased over recent years, making it a growing concern in areas where ticks are prevalent.
Transmission and Early Symptoms Powassan virus is primarily transmitted through the bite of infected ticks, most notably the same species that transmit Lyme disease. The virus can be transmitted in as little as 15 minutes after a tick bite. This short transmission time makes prevention strategies particularly important.
Early symptoms of Powassan virus can include fever, headache, vomiting, weakness, and confusion, which can develop anywhere from one week to one month after being bitten. Since the virus infects the central nervous system, more severe symptoms can emerge, such as seizures, difficulty speaking, loss of coordination, and in some cases, encephalitis (inflammation of the brain) or meningitis (inflammation of the membranes surrounding the brain and spinal cord). Early diagnosis can be difficult due to the nonspecific nature of initial symptoms, and in many cases, people may not even remember being bitten by a tick.
Progression and Long-Term Effects In severe cases, Powassan virus can lead to neurological complications, including swelling of the brain and spinal cord, long-term cognitive issues, and motor dysfunction. About 15% of those with severe cases die from the infection, and many survivors are left with permanent neurological damage. There is no specific antiviral treatment for Powassan virus; instead, care focuses on managing symptoms, including hospitalization for severe cases to provide supportive treatments like respiratory support, intravenous fluids, and medications to reduce brain swelling.
Epidemiology Powassan virus is most prevalent in areas where Ixodes ticks are found, particularly in the northeastern and midwestern United States and parts of eastern Canada. The virus has been reported in an increasing number of cases, reflecting both rising tick populations and increased awareness. Powassan virus poses a serious health threat, especially as tick habitats expand due to climate change and other environmental factors.
The Impact of Powassan Virus The health impacts of Powassan virus are profound due to the potential for severe neurological damage and death in a subset of those infected. While many people infected with the virus may remain asymptomatic or have mild symptoms, the risk of life-threatening complications makes it a critical public health concern, especially in endemic regions. Individuals who live, work, or spend time in areas with tick populations should take preventive measures to reduce their risk of exposure, including using insect repellents, performing tick checks, and avoiding high-risk areas like tall grasses or wooded regions.
Powassan Virus and Public Health Powassan virus is a growing concern in tick-endemic areas, particularly due to its rapid transmission and the potential for severe outcomes. As tick populations continue to grow and expand geographically, awareness, prevention, and early intervention are essential in mitigating the effects of this dangerous tick-borne disease.
Early symptoms often mimic common viral infections, such as the flu or West Nile virus, complicating diagnosis. Since Powassan virus can lead to inflammation of the brain (encephalitis) and the membranes surrounding the brain and spinal cord (meningitis), neurological symptoms are particularly common and can be severe. The overlap of symptoms with other tick-borne illnesses, such as Lyme disease, further complicates diagnosis in areas where these diseases are endemic.
List of Common Powassan Virus Symptoms
The symptoms of Powassan virus can vary from mild to severe, with some individuals remaining asymptomatic. When symptoms do appear, they often progress rapidly and can include neurological complications. Below is a general overview of symptoms associated with Powassan virus:
General Symptoms:
Fever
Chills
Headache
Fatigue and weakness
Muscle pain (myalgia)
Nausea and vomiting
Neurological Symptoms:
Confusion
Seizures
Loss of coordination (ataxia)
Difficulty speaking (aphasia)
Sensitivity to light (photophobia)
Stiff neck (indicative of meningitis)
Changes in personality or mood
Severe Neurological Complications:
Encephalitis (inflammation of the brain)
Meningitis (inflammation of the membranes surrounding the brain and spinal cord)
Paralysis
Coma
Respiratory Symptoms:
Difficulty breathing in severe cases
Respiratory distress
Gastrointestinal Symptoms:
Nausea
Vomiting
Abdominal discomfort (though less common)
Severe Cases Can Include:
Brain swelling
Persistent neurological deficits
Long-term cognitive dysfunction
Death (occurs in approximately 10% of severe cases)
It’s important to note that not everyone with Powassan virus will exhibit all of these symptoms, and their severity can vary greatly. In many cases, individuals may experience only mild flu-like symptoms. However, for those with more severe infections, particularly involving the nervous system, the disease can progress rapidly, leading to permanent neurological damage or death. Prompt medical attention and supportive care are crucial in managing severe Powassan virus infections.
Powassan Symptoms
Overview of Testing for Powassan Virus
Testing for Powassan virus presents challenges due to the rarity of the infection and the similarity of its symptoms to other tick-borne diseases and viral infections. A timely and accurate diagnosis is critical, especially given the virus's potential to cause severe neurological damage. The testing process usually involves a combination of clinical evaluation and specialized laboratory tests. Here is an overview of the primary methods used to diagnose Powassan virus:
Polymerase Chain Reaction (PCR) Testing
Method: PCR testing detects Powassan virus genetic material in blood, cerebrospinal fluid (CSF), or other bodily fluids.
Process: A sample is taken from the patient and amplified in the lab to detect even low levels of the virus’s RNA.
Advantages: PCR is highly sensitive and specific, making it effective for early detection of the virus.
Limitations: PCR tests are highly specialized and not always readily available in all healthcare settings. They require access to advanced laboratory equipment and expertise, and they may not detect the virus in later stages of infection.
Serologic Tests
Method: These tests measure the presence of antibodies against the Powassan virus in the blood.
Types: The most common serologic tests for Powassan include the enzyme-linked immunosorbent assay (ELISA) and indirect fluorescent antibody (IFA) testing.
Advantages: Serologic tests can detect antibodies produced in response to the infection, making them useful in confirming recent or past infections, especially when the patient presents in later stages.
Limitations: These tests can take time to turn positive, as antibodies may not develop until several days or weeks after infection. Additionally, cross-reactivity with other flaviviruses, such as West Nile or Zika, may lead to false-positive results.
IgM and IgG Antibody Testing
Method: Tests for both IgM and IgG antibodies, which help differentiate between recent (acute) and past infections.
Process: A blood sample is tested for IgM (which typically appears early in infection) and IgG (which appears later and indicates long-term exposure).
Advantages: IgM antibody tests can confirm a recent infection, while IgG can show past exposure or immunity.
Limitations: Like other serologic tests, antibody levels can remain elevated for an extended period after infection, complicating the diagnosis of a current infection versus a past one. It also takes time for antibodies to appear, which may delay diagnosis in the early stages.
Cerebrospinal Fluid (CSF) Analysis
Method: A lumbar puncture (spinal tap) is performed to collect CSF for testing.
Process: CSF is tested for elevated white blood cells, proteins, and other markers of infection, along with PCR or antibody testing to detect Powassan virus.
Advantages: This method is particularly useful for detecting neurological complications like encephalitis or meningitis caused by the virus.
Limitations: CSF analysis is an invasive procedure and is only used in more severe cases, particularly when neurological symptoms are present.
Combination Testing
Practice: In many cases, a combination of tests is used to diagnose Powassan virus, especially when results from individual tests are inconclusive or conflicting.
Rationale: Since each testing method has limitations, combining serologic tests, PCR, and CSF analysis can provide a more complete diagnostic picture, particularly in severe or complex cases.
Diagnosing Powassan virus requires careful consideration of both clinical symptoms and laboratory findings. Due to the virus’s rarity and the complexity of its presentation, multiple tests may be needed to confirm infection. Health professionals experienced in tick-borne diseases are essential for accurate diagnosis and appropriate management, especially in cases with severe neurological involvement. Early detection and intervention are critical in preventing long-term complications and improving patient outcomes.
Overview of Treating Powassan Virus
Currently, there is no specific antiviral treatment for Powassan virus, so medical care is focused on supportive treatments to manage symptoms and prevent complications. The treatment approach varies depending on the severity of the illness, with more intensive interventions required for severe neurological cases. Below is a comprehensive overview of treatment options for Powassan virus:
Supportive Care
Hospitalization
Method: Patients with severe symptoms, particularly neurological involvement, are often hospitalized for close monitoring and supportive care.
Process: In a hospital setting, patients may receive fluids, electrolytes, and medications to manage symptoms such as fever, seizures, and respiratory distress.
Advantages: Hospital care provides the resources needed to manage life-threatening complications such as brain swelling and respiratory failure.
Limitations: While supportive care is essential for managing symptoms, it does not directly target the virus itself, as no antiviral treatment is available.Respiratory Support
Method: For patients with severe respiratory symptoms or who are unable to breathe independently due to encephalitis, mechanical ventilation may be required.
Process: Intubation and mechanical ventilation assist with breathing until the patient is able to recover sufficient respiratory function.
Advantages: This can be life-saving in cases of severe respiratory failure.
Limitations: Prolonged mechanical ventilation can have its own risks, including infections and complications from immobility.
Medications
Corticosteroids
Method: Corticosteroids may be used to reduce inflammation in the brain and spinal cord in cases of encephalitis or meningitis.
Process: Administered intravenously or orally, corticosteroids help lower inflammation and prevent further damage to brain tissue.
Advantages: Corticosteroids can help reduce swelling and the risk of long-term neurological damage.
Limitations: The use of corticosteroids is debated and may not always be recommended, as they can suppress the immune system, potentially prolonging recovery.Anticonvulsants
Method: For patients experiencing seizures, anticonvulsant medications may be prescribed to control and prevent seizure activity.
Process: These medications stabilize electrical activity in the brain, preventing seizures from occurring.
Advantages: Proper seizure management is critical to preventing additional brain damage.
Limitations: Anticonvulsants may have side effects such as drowsiness or dizziness, and they do not treat the underlying viral infection.Pain Management
Method: Over-the-counter or prescription pain relievers may be used to manage headaches, muscle pain, and other discomforts caused by the virus.
Process: Medications like acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used to alleviate pain and reduce fever.
Advantages: Effective pain relief improves patient comfort and helps with recovery.
Limitations: Pain management does not address the underlying virus, and excessive use of NSAIDs can have adverse effects on kidney function and gastrointestinal health.
Long-Term Management
Neurological Rehabilitation
Method: For patients with lasting neurological deficits, such as cognitive impairment, paralysis, or speech difficulties, rehabilitation therapy may be necessary.
Process: Physical, occupational, and speech therapy can help patients regain lost function and adapt to new limitations.
Advantages: Early intervention with rehabilitation therapies can improve long-term outcomes and quality of life for patients recovering from severe neurological damage.
Limitations: Recovery from severe neurological damage can be slow and may not result in complete restoration of function.Follow-Up Monitoring
Method: Regular follow-up visits with healthcare providers are important for tracking recovery and managing any lingering complications.
Process: Neurological evaluations, imaging studies, and cognitive assessments help determine the extent of recovery and guide ongoing treatment plans.
Advantages: Consistent monitoring helps address complications early and adjust treatment as needed.
Limitations: Some patients may experience permanent damage, and follow-up care may be required for years after the initial infection.
Integrative and Supportive Therapies
Immune System Support
Method: Although no specific antiviral treatment is available, some healthcare providers may recommend strategies to boost the immune system during recovery.
Process: This can include nutritional support, supplements, and lifestyle changes aimed at improving immune function.
Advantages: A stronger immune system may aid in quicker recovery and help manage the effects of the virus.
Limitations: There is limited clinical evidence supporting the efficacy of immune-boosting therapies in treating Powassan virus specifically.
Since there is no targeted antiviral treatment for Powassan virus, management focuses on supportive care to address symptoms and prevent complications. The severity of the infection, particularly in cases involving the central nervous system, often dictates the level of care required. Patients with neurological complications may need long-term rehabilitation and follow-up care to manage persistent symptoms or deficits. Given the serious nature of Powassan virus infections, working with healthcare providers experienced in treating tick-borne diseases is essential for improving patient outcomes.